KANSAS CITY, Kan. (AP) — Anticipated staffing shortages amid surging coronavirus cases could hit rural hospitals especially hard because smaller communities have more limited options for finding providers to cover for sick workers, medical providers say.
“We are doing what we can to make sure our staff are staying healthy and safe and able to be available to treat the community, but we also have heard that with post-holiday, this could be a challenge,” said Cindy Samuelson, senior vice president for the Kansas Hospital Association. “There is lots of potential for community spread.”
About 44% of the state’s hospitals on Monday were anticipating staffing shortages this week with an expected rise in COVID-19 cases following the Thanksgiving holiday, according to the association’s COVID-19 dashboard.
“I know that in some of our communities just keeping the providers healthy is something that is an intense focus,” Samuelson said. “We have rural communities where as that number gets higher and more and more of their providers get impacted, that takes them out of service and so this challenge of finding providers to cover is increasing.”
Kansas ranks 13th in the nation with 1,210 COVID-19 cases per 100,000 residents, according to an analysis by The Associated Press of data collected by the John Hopkins University Center for Systems Science and Engineering.
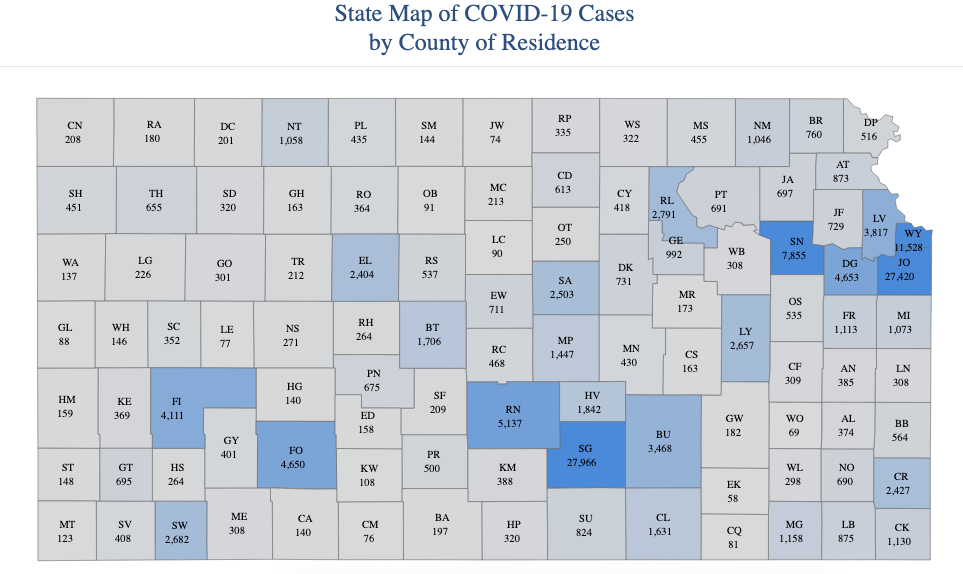
Five rural Kansas counties — Rush, Republic, Ellsworth, Rawlins and Kearny — rank in the top 25 counties in the nation with the most new cases per capita in the past 14 days.
If medical providers in rural areas get COVID-19 it “really puts small rural hospitals at risk” because options in small communities can be challenging and limited, Samuelson said.
Ben Kimball, a physician assistant at Graham County Hospital in Hill City in rural northwest Kansas, said he spent hours on the phone and had to make multiple calls to transfer out three COVID-19 patients and one without the virus from Friday through early Monday.
Two were flown to Kearny Regional Hospital in Nebraska, about 100 miles away, and the other two to the University of Kansas Hospital in Kansas City, Kansas, about 275 miles away. One of the patients had to be put on a ventilator.
“We have always been able to send people to a place with an ICU or critical care services if we needed to,” he said. “I think we are are all kind of nervous that that ability is dwindling.”
The hospital normally has just three to six in-patients at a time and doesn’t have the staffing or equipment to handle more complex cases.
“We are small to begin with,” he said. “If we get a couple nurses out or aides out, that makes a difference.”
Even some larger hospitals are struggling with rising patient numbers and staffing challenges.
The intensive care unit and the COVID-19 ward at Hutchinson Regional Medical Center are both full and the hospital’s overflow COVID ward is nearly full, The Hutchinson News reported.
There were nine people on ventilators Tuesday morning, and the hospital is running out of specialized equipment for new patients, said Chuck Welch, the hospital’s vice president.
“We’re literally down to a handful of (ventilators) and a handful of beds,” Welch said. “We’re buying everything we can get hands on, but none are available. Shortages are extending past PPE to actual physical machinery.”
The hospital also faces staffing issues with a 35 employees under observation for COVID-19, including 12 who have tested positive and 23 others awaiting test results. More than a dozen are currently working from home.
“We have what I consider, per capita, one of the best health care teams in the region,” he said. “We have four pulmonologists and a team of hospitalists,” Welch said. “For a hospital with a community population of our size, we’re better off than many bigger cities. But that’s not going to help us if we don’t wear masks and distance ourselves. ”



